How to manage difficult pleural effusions
Ramesh Kaul, MD, FCCP, FACP, Master of Surgery.
This is a practical insight to my surgery in pleural effusions.
Effusions can become difficult if the effusions are very large, or loculated, or with thick viscous exudates, with blood or with clots or recurrent in presentation.
How were we successful? What really worked ? what did not work? .
It is wise to have a non contrast CT Chest done in most of the cases, contrasts are not essential unless mesothelioma or empyema is suspected.
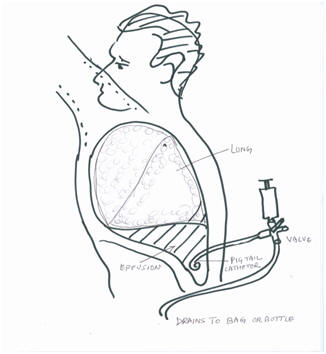
Remember lungs are inside the body cavity called thorax with shining layer of thin membrane called visceral pleura wrapped around the lungs, also another membrane(Parietal Pleura) lines the inside of the chest cavity.
There is space between the two pleural layers which is collapsed by negative pressure and thin layer of fluid.
However there can be a large amount of collection between these two layers. This causes collapse of the chest cavity. There is no space for lungs to expand and thus shortness of breath ensues.

The cascade effect of disruption of lung function leads to stress on the heart and causes heart failure.
This further pools the blood in the lungs and causes inability of lungs to inflate with air and exchange oxygen with carbon dioxide in the blood.
This is a total collapse of Heart and Lung system and may lead to death.
Early collection of fluid is reversed or prevented by shrinking the blood volume by forcing kidneys to not to absorb water back.
The net liquid loss in the blood shrinks the blood volume and thus reabsorbs the fluids back from membranes and body spaces.
The problem starts when the diuretics and fluid restriction does not work.
Choice is to tap the chest and drain the fluid with a needle catheter or a tube; this does have its risks and benefits.
The needle may cause pain, puncture the lung, cause bleeding or even fail to relieve the problem by inability to drain the fluid.
The best option is place a small pig tail catheter, and leaves it in for 24 hrs or till your next visit.